Professor Darzi is a Consultant Surgeon who was knighted for his services to medicine and surgery in 2002. He has since worked in politics where in 2007 he was introduced to the House of Lords and appointed Parliamentary Under Secretary of State at the Department of Health to lead a major review of the UK National Health Service. He was Global Ambassador for Health and Life Sciences from 2009 until March 2013.
Professor Darzi is a Consultant Surgeon who was knighted for his services to medicine and surgery in 2002. He has since worked in politics where in 2007 he was introduced to the House of Lords and appointed Parliamentary Under Secretary of State at the Department of Health to lead a major review of the UK National Health Service. He was Global Ambassador for Health and Life Sciences from 2009 until March 2013.
Professor Darzi continues to hold multiple influential roles in healthcare. He is Director of the Institute of Global Health Innovation at Imperial College London; sits as a Council Member for the UK’s Engineering and Physical Sciences Research Council; is a Non-Executive Director of NHS Improvement; is a member of Her Majesty’s Most Honourable Privy Council; holds the Paul Hamlyn Chair of Surgery at Imperial College London, the Royal Marsden Hospital and the Institute of Cancer Research; and is Executive Chair of the World Innovation Summit for Health in Qatar.
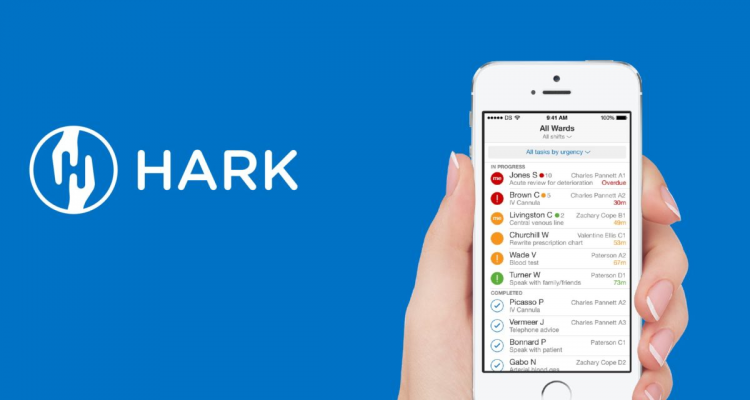
Professor Darzi is the mind behind Hark, an app recently acquired by Google, designed to help clinicians prioritise tasks.
You have some impressive credentials. What have you enjoyed most about your many-sided career?
What I have enjoyed most is just that. The variety of the challenges that I have undertaken over the past years and overseeing their development and success. I have had the privilege of meeting and working with a great number of incredibly talented and passionate individuals along the way
What is your assessment of the NHS innovation space currently?
I think that we are currently in a very exciting time, where it is widely recognised that we need to encourage and support innovation within the NHS. Having recently been a panellist at the Health and Care Innovation EXPO run by NHS England, I was delighted to see a growing awareness of the NHS innovation space.
The current focus is the development of digital technologies and there are endless opportunities for innovation in this field.
What should the NHS do to boost medical entrepreneurship and innovation over the next five years?
Innovation needs to remain a priority for the NHS. The recently published Accelerated Access Report by the Department of Health is hugely encouraging. It states that the aim is to “make the UK a world-leader in healthcare innovation, by creating flexible arrangements with innovators who are working on transformative new products.” These are the reassurances that young innovators need.
Over the past couple of years different NHS programmes have been rolled out to attract medical entrepreneurs. One such example is the NHS Innovation Accelerator, which is seeing competitive numbers of doctors applying, reinforcing that the enthusiasm and passion is out there.
What advice do you give to entrepreneurial doctors looking to improve the NHS?
Entrepreneurial doctors need to focus on the most crucial challenges of our time. One of these is the burden of chronic disease and the need to improve access to high quality, cost-effective healthcare. It’s vital that any ideas generate both health value and economic value, especially in such an economic climate as we’re in today. I have always advocated that it is crucial to ensure that patient needs are at the centre of these initiatives to empower patients to become more involved in managing their own health. I want to encourage young entrepreneurial doctors not to be disheartened. Nothing in health care is a quick fix. Change will take time, but right now is the time, so grab the opportunity.
How can junior doctors become more involved with NHS innovation?
Junior doctors are in the perfect position to join the NHS innovation scene. They are the frontline staff who see the challenges that face the NHS day-to-day. The way that training works is that junior doctors rotate through different hospitals, gaining insight into different practices and they are therefore very aware of the challenges that we face.
Junior doctors need to use this experience to develop innovative ideas and improve services. They themselves have to engage in innovation and encourage and educate patients to do so too.
If you had one week for the medical school curriculum based on your vision for the future and desire to improve healthcare, what would you put on the syllabus?
I believe that junior doctors should have an awareness that change in healthcare needs to be at system level. For this, a more comprehensive understanding of the structure of the NHS and health policy is needed.
The NHS will only face more financial pressures in the years to come and an insight into this will encourage young doctors to consider innovative ideas that generate both health value and economic value from the outset of their careers.
Junior doctors should have an awareness that change in healthcare needs to be at system level.
Congratulations on the recent acquisition of Hark by Google. What are your future plans for Hark?
Thank you. Hark – now known as Streams – is currently in the service evaluation stage with us aiming to launch the product later this year. My primary role for Hark is to ensure that the original clinical vision is delivered for the benefit of the patients and clinicians.

Hark, now known as Streams, was purchased by Google DeepMind in 2016 and is currently in the service evaluation stage.
What role do you think Google/Alphabet will play in healthcare innovation in coming years?
I believe that they will play a considerable part in healthcare innovation in the coming years. The most valuable aspect of DeepMind is that they are continually drawing on input from clinicians – all the way from medical students to longstanding consultants like myself. It is this, in combination with their direct work with patients, that will be instrumental in ensuring that healthcare innovations are diffused.
You’ve mentioned in the past that the “right business models around technology make it sustainable”. A sticking point with the current trend towards using apps to monitor chronic conditions is a lack of sustainable patient engagement. How should we address this problem?
As clinicians we are responsible for helping to educate patients about their condition and encouraging them to be engaged with their healthcare. Research has shown that patients actively involved in their healthcare tend to have better clinical outcomes. Once patients are aware of this – and it is our duty to ensure they are – they will feel more empowered to engage with these apps.
There are thousands of health apps out there. However, they crucially need to be user friendly; provide relevant, evidence-based information; and give patients autonomy.
Crucially [apps] need to be user friendly; provide relevant, evidence-based information and give patients autonomy.
Are there any healthcare start-ups that you’re particularly excited by?
A concept that greatly excites me is Imperial’s Helix Centre. This is a purpose built innovation lab which is located at St Mary’s Hospital and serves as a place for designers to collaborate with the hospital community. It aims to respond to complex healthcare issues, and turn ideas into prototype products, processes and services. It’s a hub of innovation and a foundation for start-ups to be created. They’re currently working on a range of projects including a design-led approach to improve End of Life Care.

Helix is a joint collaboration between Imperial College London and the Royal College of Art. Their multi-disciplinary team is uniquely placed on the frontline of healthcare, inside a large London NHS hospital.
Finally, if you were having a coffee with the Secretary of State for Health and Social Care, Jeremy Hunt, what would be two things you’d want to discuss?
I would want to discuss how clinicians and policy makers can best continue working together to facilitate the ongoing diffusion of healthcare innovation. I would also want to address how we can continue to meet our objectives that we laid out in our Global Patient Safety Summit last year, and how we can continue to identify the emerging threats to patient safety.